The IACFS/ME Conference I: Treatment – Lifestyle Managment, Stress Reduction, CBT and Something New



Reno, Nevada: March 12-16, 2009
By Cort Johnson
______________________________________________________________________________________________________________
Activity Management – The Crucial Element? – Energy Envelope Therapy Produces Results
A Presentation by Dr. Leonard Jason
 It’s crystal clear that there are negative consequences to pushing outside one’s ‘energy envelope’. But it’s been less clear whether the benefits of staying inside that envelope translate to more than simply ‘feeling better’. Can rigorously attending to one’s energy envelope actually improve one’s health in a measurable way? Could a sojourn inside that energy envelope actually allow some patients to recover enough energy to return to health?
It’s crystal clear that there are negative consequences to pushing outside one’s ‘energy envelope’. But it’s been less clear whether the benefits of staying inside that envelope translate to more than simply ‘feeling better’. Can rigorously attending to one’s energy envelope actually improve one’s health in a measurable way? Could a sojourn inside that energy envelope actually allow some patients to recover enough energy to return to health?
Not surprisingly, Dr. Jason is at the forefront of this question. In the last year he’s engaged in a number of fascinating studies that have examined how effective ‘lifestyle management’ programs can be and who benefits from them. In some ways his presentation may have been the most important of the conference. The WPI and others have raised hope for the future but it will take some time for their achievements to impact the ME/CFS patient on the ground. Dr. Jason is exploring issues that can affect ME/CFS patients right now.
Mind:Body? Or is it Body:Mind? In the beginning, behavioral therapists suggested that people with chronic fatigue syndrome differ little from healthy people in a physiological sense but that they’re quite different psychologically; they’re either too absorbed in their symptoms or they’re depressed or anxious – i.e., if you could just get them to stop focusing so much on their problems, they’d get well.
Dr. Jason appears to believe that those early CBT practitioners were putting the cart before the horse. Rather than the mind driving the body, it may be that the body is driving the mind. All those symptoms (that anxiety, that depression. . .) are what occur when patients transgress their physiological capabilities. His research is putting stress reduction therapies into a physiological context rather than a psychological one. Instead of suggesting that ME/CFS patients are mental basket cases he’s proposing that they’re rather courageous individuals (yes, he did say ‘courageous’) bucking up against an impaired physiology that greatly limits their choices.
He proposed that, instead of cycles of maladaptive behavior driving their limitations, there are actual physiological limits to what ME/CFS patients can achieve. Once they get outside of that activity ‘safety zone’ they encounter increased levels of oxidative stress, and neuroendocrine and immune problems that cause their symptoms to flare up again.
His thinking is clearly borne out by increasing evidence that if you push ME/CFS patients too far in any way physically or psychologically in the street or in the laboratory their systems are going to behave abnormally. (We’ll see a call go out later in the conference that all studies essentially thrust patients into a crash state before they measure them. That’s not happy news for ME/CFS patients undergoing those tests but it does indicate that the scientific community is beginning to get a critical message about ME/CFS.)
Looked at in this light, instead of correcting patient’s maladaptive thought patterns, cognitive behavioral therapies and other types of stress reduction approaches are doing nothing more than reducing stressful inputs and relieving the strain on an overworked system and allowing it to heal at least somewhat.
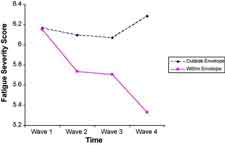 Don’t Use It – Don’t Lose It – The envelope theory is perfect for Dr. Jason’s studies. It relies on the idea that there’s only so much juice in a chronic fatigue syndrome patient’s batteries. If you use that juice up it’s gone and needs to be built up again, but if you don’t use it up it can actually build up over time. In his study Dr. Jason had chronic fatigue syndrome patients use envelope theory techniques and recorded their symptom levels. His graphs vividly showed that as ME/CFS patients use up their energy their symptoms rise dramatically. On the other hand, when they were using the energy envelope techniques not only did their symptoms drop dramatically but over time their overall level of activity increased. Here was vivid evidence that lifestyle management techniques can pay off in improved health.
Don’t Use It – Don’t Lose It – The envelope theory is perfect for Dr. Jason’s studies. It relies on the idea that there’s only so much juice in a chronic fatigue syndrome patient’s batteries. If you use that juice up it’s gone and needs to be built up again, but if you don’t use it up it can actually build up over time. In his study Dr. Jason had chronic fatigue syndrome patients use envelope theory techniques and recorded their symptom levels. His graphs vividly showed that as ME/CFS patients use up their energy their symptoms rise dramatically. On the other hand, when they were using the energy envelope techniques not only did their symptoms drop dramatically but over time their overall level of activity increased. Here was vivid evidence that lifestyle management techniques can pay off in improved health.
A Ceiling and A Floor – None of the patients were well at the end of the study but 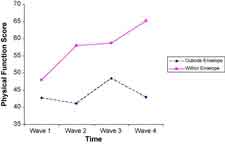 many had improved their physical activity levels by 50%. A reduction in the level of inflammatory immune cells suggested that incorporating energy envelope practices (activity/symptom logs) had reduced inflammation as well.
many had improved their physical activity levels by 50%. A reduction in the level of inflammatory immune cells suggested that incorporating energy envelope practices (activity/symptom logs) had reduced inflammation as well.
One group of patients, however, didn’t benefit significantly. This group, which appeared from their lab tests, at least, to be sicker, had increased immune dysfunction and low cortisol levels. People with normal cortisol levels found that their fatigue and anxiety decreased ‘significantly’ but those with low cortisol experienced virtually no benefit.
The authors did not speculate why low cortisol played such a fundamentally important role but it’s intriguing that low cortisol levels are found in a number of ‘stress-response’ diseases with high rates of mood disorders such as fibromyalgia, post-traumatic stress syndrome, chronic pelvic pain as well as rheumatoid arthritis, allergies and asthma.
Dig Deeper – For more on hypocortisolism and chronic fatigue syndrome (ME/CFS)
The study brings up a host of questions. Are the 30% or so of ME/CFS patients who don’t benefit much from behavioral techniques being blocked from doing so by low cortisol levels? Would hormone therapy enable them to benefit?
The study also demonstrates that energy envelope therapy can be quite effective in improving one’s quality of life and to some extent one’s health.
Dig Deeper – Energy Envelope and ME/CFS
Not Nice At All: Dr. Carruthers Takes Aim at the NICE Guidelines
Pacing as a Dynamical Embedded, Embodied Treatment/Prevention Strategy in ME/CFS. Bruce Carruthers
The UK’s NICE guidelines on ME/CFS did not endorse pacing (i.e. energy envelope techniques) even though most patients report that it works. One reason was their difficulty in defining it and the lack of research studies. (One wonders if it also conflicts with their fundamental view of this disease?) Pacing involves staying within ones energy envelope in order to avoid symptom flare-ups, to feel better, and (hopefully) to build up vitality over time.
Dr. Carruthers, one of the creators of the Canadian Consensus Definition, has, on the other hand, found PACING to be ‘an essential therapeutic strategy’ for his patients. He was obviously not happy seeing this valuable approach to ME/CFS ignored simply because the authors couldn’t define it precisely. He believes the NICE authors simply don’t get it about pacing and thus are ignoring a fundamentally important aspect of this disease.
Dr. Carruthers believes pacing is an essential strategy because the ‘delayed and prolonged’ fatigue in ME/CFS is fundamentally different from the kind of fatigue found in other diseases. Putting them rather low on the ladder of his estimation, he noted that “even the authors of the NICE Guidelines ‘ are (finally) beginning to realize this but unfortunately they still don’t fully understand what this means.”
If I understand him correctly, ‘fatigue’ is part of a complex control system. When we’re too active and our bodies are beginning to suffer, fatigue sets in and causes us to reduce our activity levels. Of course we can override this fatigue command for a time with stimulants or by ignoring it, etc. but once the command is obeyed and we become inactive, the fatigue disappears rather quickly. It’s a very easily learned behavior pattern; do too much, suffer from fatigue; obey the fatigue signal, rest and quickly recover.
That pattern, of course, has just been shredded in ME/CFS. For one, the onset of fatigue is delayed – and what a problem that causes. You can engage in an activity and feel fine and then collapse hours or even days later. Not only that, but because the fatigue state is so prolonged, it’s difficult to tell cause and effect. Was it that activity three days ago or was it something yesterday that made my symptoms so bad today? Or was it because I overdid it three days ago that this minor activity I did yesterday triggered more fatigue today? (Throw in the fact that ‘fatigue’ itself impairs our ability to understand complicated situations and you can see how difficult it is for patients to know particularly when they’re symptomatic what has caused what. )
Many patients do eventually learn how operate within this vastly new fatigue paradigm. Dr. Carruthers notes that ME/CFS patients were PACING long before NICE came on the scene. When PACING works, it works because patients figure out their own fatigue patterns and that’s something that no Top-Down strategy such as NICE can provide.
Repeat After Me “CBT Is Not A Cure….CBT Is Not a Cure….CBT Is Not a Cure….”

Response to Treatment in Chronic Fatigue Syndrome: Evaluation of Combining Cognitive Behavioral Therapy and Exercise Therapy. G. Moorken, M. Weyns, C. Mertens and H. Wyant
This ambitious and very large study (219 patients) combined the two big mainstream behavioral therapies in Europe; cognitive behavioral therapy (CBT) and graded exercise therapy (GET). One had the feeling that there were hopes that this was going to ace it for the behavioral therapists; the combination of these two hot therapies was going to knock this disease out once and for all and this large study would usher in a new era of treatment. That’s apparently what the Belgian government thought when they created a series of CFS treatment centers.
That didn’t quite happen. On the way, though, we learned some interesting things. The infectious onset cases have always got the lion’s share of attention in ME/CFS. Dr. Moorkens asked the patients in her study about triggers and, although infection was the single most common trigger, it was not deemed a trigger in most cases. Here are the triggers she identified.
• No trigger 34%
• Infection 23%
• Relational Problems 15%
• Work Related Stress 10%
• Pregnancy 9%
• Trauma 6%
• Surgery 5%
This group, with their high rates of relational violence (28%!) and their ‘hyperactive lifestyle’ (?) (30%), appeared to have a fairly high level of psychological issues and would seem to be a good candidate group for cognitive behavioral therapy. But while the participants in general improved, they didn’t improve that much and the trial failed to produce ‘significant’ benefits an apparently devastating outcome not just for the patients but for the Belgium government. Even though Dr. Moorkens told them CBT was not a cure before the trial started, they apparently didn’t take it to heart. They thought, since they thought the disease to be a psychological disorder, that the trial would succeed. They’re so upset in fact that they’re considering pulling the plug on the whole effort. (Talk about behavioral problems…..)
It’s Definitely Not A Cure…

Cognitive Behavioral Therapy for Chronic Fatigue Syndrome: A Descriptive Study of the Patient’s Perspective – Dr. Elke Van Hoof.
The conference was not a bright shining moment for CBT. Voices in the patient community have always railed against the idea of CBT being the answer to this disease but lately we’ve been hearing notes of dissension even from some CBT practitioners. The practice they say has been over-hyped: while outcomes are generally positive they also tend to be modest and the downside of the therapy is usually ignored. Patients in CBT studies have complained that they don’t recognize themselves when they read the study results. Dr. Friedberg, a psychologist and author, recently penned a critique that suggested that many of CBT’s benefits may derive simply from lifestyle readjustments. One wonders if CBT has finally reached its high water mark.
Dr. Van Hoof, a clinical psychologist in Belgium (and winner of the 2007 conference Young Investigator Award), very happily employs CBT and other behavioral therapies in her practice but even she’s had enough of the CBT mania. After all the patient complaining, she did an online survey to try to learn what patients’ experiences of these studies really were. She found that only 25% of the people who responded to her survey ended up completing the CBT course they were in. Most dropped out because the physical demands of the therapy were too great. Of her group, two percent recovered, 30% improved, 30% saw no change and 38% got worse. While some patients’ quality of life did improve always an important factor their activity levels – an even more important factor – did not.
But If Stress Management Techniques Are Done Correctly They Can Definitely Help Phoning It In In Florida
Calling in Cognitive Behavioral Stress Managment for Chronic Fatigue Syndrome – Michael Antoni
 From the beginning, the Americans appear to have had a more sophisticated approach to behavioral therapies. The hard core CBT craze which involved pushing patients through their ‘false beliefs’ – doesn’t seem to have caught on in the States. Government funded research in the US has always been more physiologically than psychologically focused. In Europe, government funded research is almost entirely psychologically oriented.ected in ME/CFS – natural killer cells – are also the immune cells that are most affected by stress.br />
From the beginning, the Americans appear to have had a more sophisticated approach to behavioral therapies. The hard core CBT craze which involved pushing patients through their ‘false beliefs’ – doesn’t seem to have caught on in the States. Government funded research in the US has always been more physiologically than psychologically focused. In Europe, government funded research is almost entirely psychologically oriented.ected in ME/CFS – natural killer cells – are also the immune cells that are most affected by stress.br />
One wonders, in fact, if any disorder that impacts the neuroendocrine and immune systems wouldn’t benefit from practices that use the mind to reduces stress and thus improve the functioning of those systems. Dr. Antoni in fact began off his talk bynoting that CBT has proven effective in improving immune functioning in HIV-AIDS and other diseases.
Dr. Antoni’s goal was to use stress management techniques (he called his therapy cognitive behavior stress management (CBSM)) to reregulate the stress response (HPA axis) and thereby improve immune functioning. He used two techniques cognitive behavioral therapy to improve coping skills, cognitive ‘appraisals’, etc., and relaxation therapies such as progressive muscle relaxation, breathing exercises, mindfulness meditation and visualization to reduce stress.
Because he had found that the physical difficulties in traveling played a large role in the high drop-out rates in CBT studies, the program was done over the telephone.
Importantly, he found that patients with more symptoms had greater levels of pro-inflammatory cytokines and reduced cortisol output; i.e., he had a physiological explanation for their symptoms. In contrast to traditional CBT trials, adherence was excellent and most patients finished the course. Unfortunately I’ve lost the results (!) but my impression was that the trial was a success, i.e., that both the patients’ self-report and laboratory measurements improved. We’ll certainly hear about this study more. Dr. Antoni received the Nancy Klimas M.D. Research Excellence Award at the Conference.
Something New – Neurolinguistic Reprograming/Meditation and Mindfulness = ‘Behavioral’ Therapy on Speed?

The Amygdala Retraining Techniques May Improve Outcomes for Patients with Chronic Fatigue Syndrome: A Clinical Audit of Subjective Outcomes in a Small Sample. Ashok Gupta MA, MSc
A few patients have claimed amazing recoveries through the use of two new neurolinguistic reprogramming programs, the Amygdala Retraining and the Lightning Process. Do these types of programs constitute the ‘next step’ in the evolution of mindfulness therapies in this disease? Ashok Gupta’s focus is not on changing beliefs per se but in repairing an injury which he believes has occurred in the brain.
Ashok Gupta believes that a ‘traumatic’ neurological event (infection, etc.) causes the fear center of the brain the amygdale to become hyper- sensitized to negative symptoms in the body. Since the amygdale turns on the ‘fight or flight’ response which leads to more negative symptoms and therefore further activation of the amygdale – this process could lead the body to get locked into a chronic fear response. Since the amygdale operates on the subconscious level the process goes on, for the most part, below our levels of consciousness. All one is left with is exhaustion and continual turmoil in the body.
The way out of this is to rebuild what Gupta calls a ‘safety neurone’ from the prefrontal cortex which controls the amygdala to the amygdala. This allows the prefrontal cortex which is involved in decision making and other complex cognitive activities to turn off the amygdale. Interestingly, several studies have found reduced grey matter volume in the prefrontal cortex. The Amygdala Retraining (AR) Process uses neurolinguistic reprogramming and meditational techniques to strengthen the prefrontal cortex and dampen down the over-active amygdala .
The study involved 37 patients who had been ill for an average of 10 years. It involved weekly or biweekly phone calls with Ashok Gupta for six months. Participants were required to do the AR process and at least 30 minutes of sitting meditation a day.
Ninety percent of the participants reported improvement with a remarkable 66% reaching full functioning (where full functioning is defined as being 80-100% of pre-illness levels) (!); these people stated that they did not believe they were suffering from ME/CFS anymore. Just over half reported they’d achieved 90-100% of their pre-illness state. Many did not experience post-exertional malaise after a moderate workout at the gym.
These were remarkable findings. The participants no doubt benefited from the personalized attention from Ashok Gupta, a former ME/CFS patient himself who noted that it was important ‘to personalize the combination of tools and techniques to facilitate the best outcomes for that patient’. Ashok Gupta has created an amygdale retraining DVD set that some patients have reported considerable success using. He’s been contacting researchers and physicians in an attempt to get a full-blown, statistically rigorous treatment trial produced. Assuming he can get that done no easy task at some point we’ll have a good strong statistical look at the efficacy of the Amygdala Retraining program.
Dig Deeper! Check out an interview with Ashok Gupta at the IACFS/ME Conference
Seeing Your Way Healthy Slowly?
 The Influence of EMDR and BioFeedback on the Hypervigilance in CFS – Dr. Elke Van Hoof
The Influence of EMDR and BioFeedback on the Hypervigilance in CFS – Dr. Elke Van Hoof
Eye movemEye movement desensitization and reprocessing (EMDR) is a neurocognitive technique designed to downregulate the fight or flight (sympathetic nervous system) response that several studies have shown is upregulated in chronic fatigue syndrome. Dr. Van Hook believes that ‘dysfunctional cognitions’ or negative patterns of thinking that get locked in in ME/CFS patients (or one would think any chronic illness) further burden their stress systems. These techniques appear to directly affect the limbic system which researchers almost from day one have associated with this disease.
Dr. Van Hook noted that everyone, healthy and unhealthy, has these negative thought patterns. It was difficult to tell if she thought ME/CFS patients had more of them than normal or if they affect ME/CFS patients more than normal. (A recent study showed that picturing a negative event affected chronic fatigue syndrome patients physiologically more than it did healthy controls. This suggests that if ME/CFS patients’ bodies aren’t already in the throes of a stress response then they’re likely teetering on the edge of one.)
EMDR is a way of breaking up negative thought patterns allowing the mind and body to relax and toning down or turning off the fight/flight response. Interestingly it does this by distracting the limbic system thus pushing it out of its aroused state.
Small Wins – On a personal note I’ve found that ‘distraction’ – which I prefer to think of as ‘re-focusing’ – can at times work very well. When I feel my body get ‘aroused’ if I refocus my attention on something different; the way my hands feel, the touch of a finger on a surface, the sounds around me etc., at times I notice the arousal in my body dinimish. ‘Distraction’ sounds like a puny technique but it’s powerful enough that some pain researchers describe it as the most effective means of reducing the most challenging symptom of all severe pain.
Dig Deeper: Dr. Lasich on ‘the most powerful pain reliever in the world”.
When you’re distracting yourself you’re doing more than just diverting your attention. Brain researchers have shown that every time you use your brain in a new way neurons start to grow in a new area of the brain. If I distract myself by running my fingers across a surface near me then the touch area of the brain will become highlighted. At the same time, that area of the brain that was aroused will calm down and the neurons that feed it will start to drop away. This process is called neural remodeling. Neural remodeling is what allows stroke victims who undergo proper training to regain functioning.
Dr. Van Hook believes that ‘hypervigilance’ or state of nervous system ‘arousal’ in ME/CFS is the body’s attempt to rebalance the parasympathetic (rest and digest) and sympathetic (fight or flight) systems. Interestingly, given Ashok Gupta’s theory, she noted that these types of therapies are hypothesized to reduce amygdala activation. (The amygdala is the ‘fear center’ of the brain and it was referred to several times during this conference.)
(The idea that ME/CFS patients are in a state of ‘arousal’ has antecedents going back to the earliest descriptions of this disease. Several early accounts of myalgic encephalomyelitis comment on the emotional components of the disease with some alluding to a strange kind of ‘nervous tension’ that often accompanies it. )
Dr. Van Hook did not find that EMDR reduced sympathetic nervous system functioning but she did find that it produced significant improvement in fatigue, concentration, vitality and most importantly what’s called ‘role physical’. Because role physical measures how much activity one can maintain it’s one of the more important self-report tests used. We don’t know how much improved these patients were we’ll have to wait until Dr. Van Hook’s paper comes out.
I briefly talked to Dr. Van Hook. She was very high on this procedure, stating that although it was a very slow process, over the period of two years she’d had several patients return to full health. This kind of fits with my experiences with the Amygdala Retraining process and other meditative pursuits; while progress may be very slow it does appear to be cumulative over time. (Ashok Gupta stated that EMDR was very similar to a technique used in his Amygdala Retraining program called ‘soften and flow’. )
Dr. Van Houcke did say that she does not suggest patients try this technique on their own. She said that she didn’t believe that they needed a psychologist to monitor them but they do need a good coach (whatever that is!). It was unclear to me if this was because they can get worse doing it or because they don’t do it correctly. In any case there are different views on this matter; just an hour before she gave her talk, Dr. Friedberg who has written a book promoting EMDR’s use in FM patients gave his talk.
Dig Deeper! Check out an interview with Dr. Friedberg
Dig Deeper! For More Reno IACFS/ME Conference Overviews
- Treatment Section Part II
- The Hit of the Conference” The Whittemore-Peterson Neuro-immune Institute
- Surprise of the Conference
- Whack Those Patients – The Exercise Studies
- Rocking the Conference – Rocking the Research World: Dr Suzanne Vernon at the Mic
