 In this three part series we look at the Light’s exciting work at the University of Utah on ME/CFS. First – we look at the Light’s attempt to validate their gene expression findings, then we examine what they believe may be ground zero for ME/CFS, and finally we tie together their findings with a theory paper by Shapiro suggesting that different kind of herpesvirus may be a work in ME/CFS. Thanks to the Lights and Judith Shapiro for their willingess to answer questions and, as always, to Dennis for his invaluable help getting the research papers.
In this three part series we look at the Light’s exciting work at the University of Utah on ME/CFS. First – we look at the Light’s attempt to validate their gene expression findings, then we examine what they believe may be ground zero for ME/CFS, and finally we tie together their findings with a theory paper by Shapiro suggesting that different kind of herpesvirus may be a work in ME/CFS. Thanks to the Lights and Judith Shapiro for their willingess to answer questions and, as always, to Dennis for his invaluable help getting the research papers.
- Part I – Bad Reception? The Light Gene Expression Studies
- Part II – The Dorsal Ganglia – Ground Zero for ME?
- Part III – Varicella Zoster Virus, Shingles and ME/CFS – A New Herpesvirus for ME
- Part IV – Pts. I/II/III Combined – the Quickie Version
The Dorsal Ganglia – Ground Zero for ME?
Background: the Lights have validated unusual levels of receptor activity on the white blood cells of people with ME/CFS after exercise. The receptors involved suggest that several systems that are responsible for producing pain and fatigue have become overly activated after even moderate levels of exercise in people with CFS. The question now is what is causing these receptors to go bananas. Are they dysfunctional or are they responding to muscle damage or both?
The Cause/Causes Of CFS?
Dr. Light said it appears that the body is pumping these receptors out and they appear to be everywhere – primed to go off on a hair trigger.
She noted that the matter of “how patients actually get to the point where their system is on such a hair trigger that something that shouldn’t induce an inflammatory response – like exercise – does induce one” is still unclear but she had some ideas.
 Essentially what she and other researchers in other areas are looking for is some sort of a switch which flips a system into suboptimal state. Dr. Vernon has produced a model of a suboptimal but fixed state of functioning in the HPA axis. Dr. Kelley believes he may have a key short circuit site that keeps depression active in people with that disorder, and Dr. Light is looking for the same sort of process that gets locked in in ME/CFS.
Essentially what she and other researchers in other areas are looking for is some sort of a switch which flips a system into suboptimal state. Dr. Vernon has produced a model of a suboptimal but fixed state of functioning in the HPA axis. Dr. Kelley believes he may have a key short circuit site that keeps depression active in people with that disorder, and Dr. Light is looking for the same sort of process that gets locked in in ME/CFS.
She noted that researchers can create long lasting chronic pain and inflammatory states in laboratory animals by infecting them with something AND stressing them out at the same time. Simply stressing the animal doesn’t do it and simply infecting them doesn’t either – but doing both at the same time does.
(One way they do this is to expose animals to alternating heat and cold states. Animals can tolerate increased heat OR increased cold – but move them back and forth between heat and cold for three days – and then inject them with a pathogen – and something in their system breaks and they will lapse into a chronic pain state. It’s as if they can’t find ‘normal’ again.
 Heart Rate Variability – The low heart rate variability (HRV) findings in ME/CFS perhaps provide an intriguing analogy of a kind of frozen system. Heart rate variability tests examine the electrical signals in the heart to track the ability of the autonomic nervous system to respond to changes in the body. High HRV readings demonstrate a healthy and responsive system. People with ME/CFS, however, invariably have low HRV readings. I asked if those readings might reflect a kind of frozen system.
Heart Rate Variability – The low heart rate variability (HRV) findings in ME/CFS perhaps provide an intriguing analogy of a kind of frozen system. Heart rate variability tests examine the electrical signals in the heart to track the ability of the autonomic nervous system to respond to changes in the body. High HRV readings demonstrate a healthy and responsive system. People with ME/CFS, however, invariably have low HRV readings. I asked if those readings might reflect a kind of frozen system.
Dr. Light said they might, in a way, saying, “ the sympathetic nervous system says, I’m sorry I just have to be on overdrive all the time … I’m hypervigilant … and that can be created by conditions that are changing all the time.” It’s perhaps worthwhile, here, to recall Dr. Baraniuk’s theory of information overload caused perhaps by a breakdown of the gates that filter information to the brain in ME/CFS and fibromyalgia. High levels of pain and fatigue receptors that are primed to go off at the slightest touch suggest a certain type of information overload may exist in ME/CFS – an overload that could perhaps cause a system to be unable to return to normal.
But Where Does it All Start– Rather provocatively, Dr. Light asked “are we studying (i.e. seeing) the cause of ME/CFS or the effect?” The answer was that she does not believe that this plethora of upregulated receptors – which are surely sending the nervous system into a tizzy – are the cause of ME/CFS at all. They are simply reflect damage elsewhere and she thinks she knows where this damage is occurring: a part of the nervous system called the dorsal root ganglia.
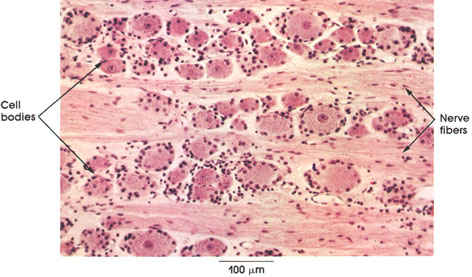
 The Dorsal Root Ganglia
The Dorsal Root Ganglia
Found just outside the spinal cord, the dorsal root ganglia are basically the last stops for sensory nerve traffic before it reaches the spinal cord. They contain bundles of nerve cell bodies which reach long nerve strands into the skin, muscles and organs of the body. From there these nerve strands send a constant stream of information about the functioning of the body into the spinal cord and then into the brain.
Dr. Light believes that something in the dorsal root ganglia has caused the wrong messages to be sent to the brain in ME/CFS … and she is not alone.
The Cry Wolf Syndrome Hits the Dorsal Ganglia – the Lights don’t just believe that the fatigue and pain symptoms in ME/CFS are the result of the brain responding to faulty information from the DRG; they believe that damaged neurons in the DRG are actually interfering with proper autonomic nervous system functioning.
They believe the DRG neurons have ‘cried wolf’ a few too many time for the sympathetic nervous system. The body cleans out the ‘garbage products’ produced during exercise by flushing the muscles with blood. In CFS patients the upregulated ANS receptors have essentially been screaming (crying wolf) for the body to send more blood to the tissues to clean up the damage in the muscles. The problem is that our nervous system tends to stop listening to signals that never change. It may be that its seen that message too many times and in what it believes to be inappropriate circumstances (mild exercise) and it’s simply decided to ignore it…..Now instead of your sympathetic nervous system sending blood to your muscles after or during exercise – it just shuts down – setting the stage for more trouble.
 Muscle Acidosis and Metabolic Problems And Nerve Problems?….. Yes! – The Newton studies have revived the idea of increased acidosis and metabolic problems in the muscles in people with CFS – a topic that had faded in interest after several studies found no evidence for it. Dr. Newton, however, has been looking carefully and she’s found evidence of metabolic problems in about half of her study participants.
Muscle Acidosis and Metabolic Problems And Nerve Problems?….. Yes! – The Newton studies have revived the idea of increased acidosis and metabolic problems in the muscles in people with CFS – a topic that had faded in interest after several studies found no evidence for it. Dr. Newton, however, has been looking carefully and she’s found evidence of metabolic problems in about half of her study participants.
The Light’s initial finding appeared to suggest that the problem was all in the nerves but the body is much more complex than that. The Newton finding of increased muscle acidosis actually may fit glove in hand with the Lights works. Dr. Alan Light stating that “We were very happy to see the results that Newton and Jones and their colleagues have been publishing. It is really nice work”.
The Lights believe that that shut down sympathetic nervous system we were just talking about is impairing blood flows to the tissue which allows the metabolites produced during exercise to build up resulting in muscle acidosis. Dr. Newton found increased acidosis in about half of her study participants but Alan Light thinks it’s possible that its present in most patients but only shows up easily in a subset of them and that it will take longer bouts of moderate exercise for their type of acidosis to show up.
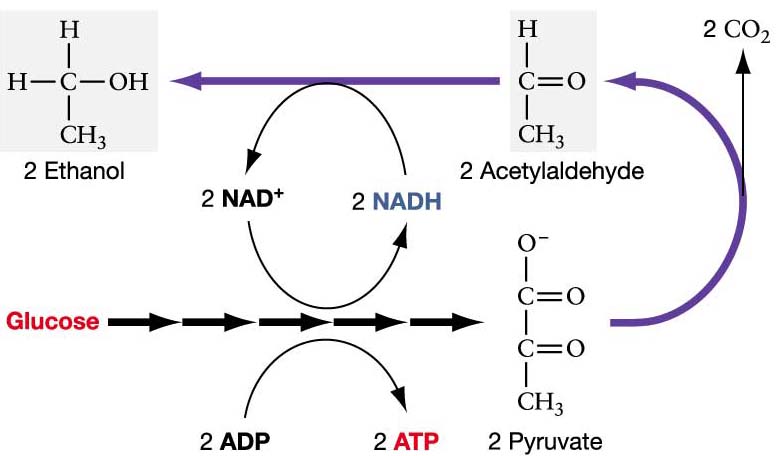 Reduced blood and oxygen flows to the muscles and reduced metabolite disposal add up to a condition called ischemia which is associated with high levels of oxidative stress. I asked Dr. Light if his DRG/sympathetic nervous system scenario could explain the quick entry to anerobic energy production seen in the Pacific Fatigue Lab and other studies using the Stevens exercise protocol or the Fulle or Jammes studies suggesting problems with energy production and oxidative stress during exercise. In a word he said “Yes, it could account for all of them’ but that the jury is still out on the role the mitochondria play.
Reduced blood and oxygen flows to the muscles and reduced metabolite disposal add up to a condition called ischemia which is associated with high levels of oxidative stress. I asked Dr. Light if his DRG/sympathetic nervous system scenario could explain the quick entry to anerobic energy production seen in the Pacific Fatigue Lab and other studies using the Stevens exercise protocol or the Fulle or Jammes studies suggesting problems with energy production and oxidative stress during exercise. In a word he said “Yes, it could account for all of them’ but that the jury is still out on the role the mitochondria play.
It’s always lovely to see study findings fit together but the plot gets even more interesting when our old friends the herpesviruses show up.
A Reservoir for Guess What . . . Herpesviruses – In 2009, a Medical Hypotheses Journal article by psychologist Judith Shapiro proposed that the primary site of infection in ME/CFS is not the central nervous system or white blood cells but the dorsal root and other peripheral ganglia. (Both the dorsal root and the other peripheral ganglia are found outside of the central nervous system. The DRG’s carry sensory nerve information, other peripheral ganglia carry autonomic nervous system information.)
Shapiro argued that placing a herpesvirus infection in ME/CFS in these nerve cell centers would make a lot of sense because:
- The Location Makes Sense – Shapiro’s theory places these viruses in a location that has reduced defenses against the kinds of viruses found in ME/CFS. Researchers have long pondered whether central nervous system viruses play a role in ME/CFS but the blood/nerve barrier in the dorsal root ganglia provides fewer protections against viruses than does the blood/brain barrier and may be a more likely candidate for infection. Indeed, Shapiro states the DRG are ‘uniquely vulnerable’ to herpesvirus infections.
 It Makes Sense of the High distress/Low fatality rate in ME/CFS – people with ME/CFS do die but perhaps not nearly as often as one would suspect given how ill much of the population is. The low death rate, Shapiro says, has contributed to the perception that CFS is primarily a psychiatric disorder. A debilitating but not fatal illness is precisely the type of illness one would predict would occur, however, from an infection found in the peripheral ganglia. These infections could be debilitating and could ultimately lead to death but their location outside the brain should keep fatality rates low and distress levels high.
It Makes Sense of the High distress/Low fatality rate in ME/CFS – people with ME/CFS do die but perhaps not nearly as often as one would suspect given how ill much of the population is. The low death rate, Shapiro says, has contributed to the perception that CFS is primarily a psychiatric disorder. A debilitating but not fatal illness is precisely the type of illness one would predict would occur, however, from an infection found in the peripheral ganglia. These infections could be debilitating and could ultimately lead to death but their location outside the brain should keep fatality rates low and distress levels high.- Difficulty in Detection – The peripheral and dorsal root ganglia also presents a barrier to detection as nerve tissue is largely separate from the general circulation with virus detection often requiring a specialized autopsy, which is not often done. Shapiro noted that Sophia Mirza’s autopsy revealed abnormalities in the sensory ganglia similar to those found in shingles (VZV).
- Accounts for Symptoms Well – Shapiro believes infection of autonomic nervous system ganglia may be causing the sympathetic nervous system activation (fight or flight response), HPA axis and sleep problems and, perhaps importantly, could cause the post-exertional malaise or relapse seen after exercise. Infected sensory (DRG) nerve ganglia, on the other hand, could account for the muscle pain and burning, numbness and tingling, vertigo and overstimulation by lights, sounds and odors, etc.
Dr. Alan Light agreed that Shapiro’s theory had merit stating
Dr. Vernon has stated that ME/CFS could be all about ‘signaling’ and this is what we’re getting into here. The scary thing about this scenario is that most of the bad stuff really is mostly hidden from view. In this model you and your blood results appear to be mostly fine (aka its all in your head) but your nervous system – which is hard to pin down – thinks not. This is not to say that the body is not being effected; the high levels of oxidative stress, NK cell problems, herpesvirus reactivations, low blood volume, muscle acidosis, etc are all there but a big chunk of the puzzle is obviously still missing. A hypersensitive receptor network that turns even normal signals from the body into a disaster would fill in the picture well.
Light and Shapiro are not alone in their interest in the connection between herpesviruses, and the dorsal root ganglia. Earlier in 2009 Martinez-Lavin, a fibromyalgia researcher, called the DRG a ‘reservoir’ for latent herpesviruses as well as enteroviruses, borrelia (Lyme) and HIV. He noted that trauma or infection can cause the over-expression of sympathetic nervous system fibers and sodium channels in DRG that researchers know lead to increased pain. Whatever the cause, all three groups are looking to the DRG to explain the fight/flight (sympathetic nervous system) and other problems in CFS.
The Shapiro article does not appear to have attracted much attention to date, but one wonders if, as the Lights proceed, it will.
 Another Player – Over-active Immune Cells in the Brain (the Microglia) – The Lights believe that immune cells in the brain and spinal cord called the microglia may also play a role. Those P2x receptors that went off like a skyrocket in people with ME/CFS after exercise also just happen to show up in spades in the microglia of mice which have been pushed into exercise-induced pain states.
Another Player – Over-active Immune Cells in the Brain (the Microglia) – The Lights believe that immune cells in the brain and spinal cord called the microglia may also play a role. Those P2x receptors that went off like a skyrocket in people with ME/CFS after exercise also just happen to show up in spades in the microglia of mice which have been pushed into exercise-induced pain states.
Microglia are immune cells present in large numbers throughout our central nervous systems. Like most immune cells, they usually maintain themselves in a resting state, and are activated by an injury or an infection. At the State of the Knowledge Conference on ME/CFS, Dr. Kelley noted that the switch that turns an inflammatory incident into a chronic depression appears to happen in the microglia.
The same thing could be happening in CFS and those upregulated P2X receptors could be involved.
Heredity Kicks In? The COMT Gene Findings – There’s been lots of anecdotal evidence that CFS tends to run in families but until recently there’s been little hard evidence. A recent study by the Lights and Dr. Bateman, however, provides strong evidence that it does and the Lights other studies may be showing how…one of the upregulated genes they’ve found has been implicated in CFS by two other research groups using different methods.
Thus far three research groups (CDC 2006, Wyller 2011, Lights 2009/11) have found abnormalities in either COMT gene expression or COMT gene makeup in people with ME/CFS. The 2011 Wyller study linked COMT gene alterations (rs4860) in adolescents with increased sympathetic nervous system (‘fight or flight’) activity and both Light studies have shown increased expression of the COMT genes after exercise.
The COMT (Catechol-O-Methyl-Transferase) Gene – In some ways COMT is a perfect gene for CFS and FM because it degrades the ‘fight or flight’ hormones (eg catecholamines norepinephrine/epinephrine) released by the adrenal glands during stress. A balky COMT gene, then, could contribute to the increased sympathetic nervous system activity several studies have found is present in CFS.
Dr. Light noted that they started looking at the COMT gene after a colleague found that it was a risk factor for TMJ and FM and they were surprised at the degree of dysregulation they found in CFS. They believe (and are still not sure) that it may be a risk factor for CFS.
The Ultimate Cause? – The ultimate cause of these receptor blowups is probably going to be a combination of factors – genetic, viral, environmental….that combine together to throw a persons system into disarray and be unable to find ‘normal’ again. The good news is that all known causes of the kind of receptor malfunction that appears to be occurring in ME/CFS fit within standard CFS paradigms: viral infections, chronic stress, nerve injury and genetic susceptibility all are suspected in ME/CFS.
THE NEXT STEP
Testing the theory -The Lights theory predicts they will find the same receptor upregulation on neurons in the dorsal root ganglia that they are finding in the white blood cells and this is what they’ll be testing next. They can’t actually manipulate the DRG – that’s a dangerous procedure that can cause long lasting pain but they can drop muscle metabolites (such as lactate, ATP) into muscles and then determine if they get the same response they’ve seen after exercise. If the receptor levels shoot up again in the ME/CFS patients they’ll have directly shown that the systems of people with ME/CFS respond abnormally even to small amounts of ATP or lactate (or whatever substances they use.) Because the muscles are enervated with neuron fibers emanating from the DRG a positive finding will point to the DRG and ultimately, hopefully, the recognition of ME/CFS as a neuropathic disorder. Several years ago Dr. Natelson speculated that overactive sensory nerves in the muscles may be causing the pain and fatigue in ME/CFS.
I asked Dr. Light if he could show that receptor levels in the DRG neurons in CFS and FM are significantly altered relative to controls – would that be enough for drug companies to put money into producing drugs targeted for those receptors? He said “We certainly hope so!”
Support Phoenix Rising