 Kim McCleary stated that the Alter paper was the most anticipated research paper on ME/CFS ever and she was surely right. Demonstrating a remarkable online viral spread of its own Kim reported over 150 media outlets quickly jumped on the XMRV story. The story sent attendance at the Phoenix Rising Forums zooming, quickly breaking the record for online attendance and then breaking the Forums themselves, knocking them off-air for about 30 minutes.
Kim McCleary stated that the Alter paper was the most anticipated research paper on ME/CFS ever and she was surely right. Demonstrating a remarkable online viral spread of its own Kim reported over 150 media outlets quickly jumped on the XMRV story. The story sent attendance at the Phoenix Rising Forums zooming, quickly breaking the record for online attendance and then breaking the Forums themselves, knocking them off-air for about 30 minutes.Validation…Vindication – We believed that the findings would validate the WPI’s results and, proving, once again that nothing is easy in chronic fatigue syndrome, they both did and they didn’t. They did in the most important sense; the Alter/Lo study (Lo was the principal investigator) confirmed the major finding of the original Science paper– that retroviruses are highly prevalent in people with CFS and are found in much lower levels of the general population. After all the zeros and null findings of the previous studies, the Alter findings were remarkably consistent with the WPI’s original findings (86% of CFS patients vs 68% and 7% of controls vs 4%). The fact that two accomplished researchers using their own samples and their own techniques duplicated the finding of mouse retroviruses in chronic fatigue syndrome was enormously beneficial.
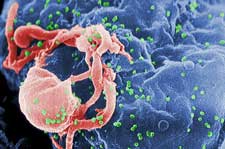
As if to demonstrate that there’s always room to get weirder in CFS they were unable to find XMRV. Instead, they found a mélange of its closely related cousins – the murine leukemia retroviruses (mLV’s) – suggesting that instead of one retrovirus we’re looking at possibly four.
So how did they find these new retroviruses? The genetic sequences Lo and Alter looked for during the first pass of nested PRC were the same as the genetic sequences that all the other studies looked for. The Lombardi (WPI), Groom, McClure and Switzer (CDC) papers all looked for ‘gag’ sequences identified by primer #’s 419F/1154R. The Alter/Lo group, however, used different primers for the second round of the PCR. The Alter study used sequences that were more similar to those the WPI used for its second round. (It does not appear to explain why the Alter group was able to get 50% positives during the first round of PCR).
Right On Track – At this point the Lo/Alter group was right on the mark with the WPI – both had found that a high proportion of their CFS samples tested positive for that sequence. The gag sequence they identified, however, is not specific to XMRV – it is a marker for a range of murine leukemia retroviruses of which XMRV is one. Hence, both groups did a phylogenetic analysis to determine exactly what viruses they had identified; first they amplified the sequence in order to flesh it out, and then they compared it to other known retroviruses and here was where the two studies diverged.
 The Alter/Lo group discovered they had not found XMRV at all; instead they had uncovered four of its close cousins (96.6% similarity). While XMRV lacks the genetic sequences it needs to infect mice, these retroviruses had them -instead of xenotropic MLV’s they were polytropic MLV’s able to infect mice and other mammals. (Tropism refers to the types of tissues or organisms a pathogen can infect). Although three MLV’s were found one MLV dominated the rest, infecting 86% of the CFS patients. One of the MLV’s was found also in one healthy control.
The Alter/Lo group discovered they had not found XMRV at all; instead they had uncovered four of its close cousins (96.6% similarity). While XMRV lacks the genetic sequences it needs to infect mice, these retroviruses had them -instead of xenotropic MLV’s they were polytropic MLV’s able to infect mice and other mammals. (Tropism refers to the types of tissues or organisms a pathogen can infect). Although three MLV’s were found one MLV dominated the rest, infecting 86% of the CFS patients. One of the MLV’s was found also in one healthy control.
An accompanying commentary “Mouse Retroviruses and chronic fatigue syndrome: Does X (or P) mark the spot?”) indicated the MLV’s, of which XMRV is one, are a quite intermingled group. A major part of the XMRV genome, for instance, is simply a compilation of various MLV sequences. This kind of ‘cross-dressing’ or pseudotyping commonly occurs in the MLV’s and is believed to play a key role in their ability to infect new species.
One genomic element, in fact, the ‘glycogag’ section, has been shown to have the ability to jump species. Glycogag incorpation into HIV-1 enhances it’s production and the incorporation of this MLV sequence into other retroviruses and perhaps even viruses could enhance their pathogenicity. Dr. Sandra Ruscetti, an MLV expert, is reportedly currently focusing her research on this subject.
Finally A Retrovirus That Acts Like a Retrovirus! – The variability the Alter group uncovered was actually good news to them. The high genetic homogeneity initially attributed to XMRV by the WPI was disturbing because retroviruses, including murine retroviruses, usually mutate quickly and often combine together to form new combinations. Finding the small swarm of murine retroviruses provided further evidence to the Alter/Lo group that the retroviral presence in ME/CFS was real. (The small sample size of the WPI’s phylogenetic analysis- 3 samples – could have contributed to the low genetic variability reported).
 What about XMRV? – What is going with XMRV itself is not as important as it was before the Alter paper but it is still an unresolved question. Dr. Alter was quick to point out that the WPI initial findings and the overlapping evidence they presented were still far beyond what any other group had accomplished. Not only did they find the virus but they cultured it (Dr. Lo is working on that now), showed it could infect other cells and demonstrated an immune response had formed to it.
What about XMRV? – What is going with XMRV itself is not as important as it was before the Alter paper but it is still an unresolved question. Dr. Alter was quick to point out that the WPI initial findings and the overlapping evidence they presented were still far beyond what any other group had accomplished. Not only did they find the virus but they cultured it (Dr. Lo is working on that now), showed it could infect other cells and demonstrated an immune response had formed to it.
While the WPI’s overall thesis was confirmed we still apppeared to have two disparate findings; the WPI found XMRV and no other MLV’s while the Lo/Alter group found no XMRV and several other MLV’s. Researchers abhor impasses like this and they must eventually be cleared up. That the virus is exceedingly tricky is clear.
It’s possible but hardly likely that both findings are correct. If retroviruses are usually found in’ swarms’ even within the same person’s body then it seems more likely that both groups are missing part of the swarm. Dr. Alter reported, in fact, that WPI researchers were finding more variation over time.
Update: The Swarm at the WPI – it’s turned out that the finding of a ‘swarm’ of viruses, all very closely related to XMRV was not news to the WPI at all. In March they published an abstract at a Cold Harbor conference indicating there were variants and they reportedly provided information on variants to the editors of Science as proof against contamination. Their antibody test picks up all the variants and distinguishes two of them – which suggests that there may be two real ‘variants’ and two forms that have synonymous amino acid alterations…ie they have a varied but functionally similar amino acid composition. In a Q & with the CFIDS Association she reported that most patients contain both polytropic (MLV’s) and ecotropic (XMRV) viruses.
Off on the Wrong Foot? – In a video Dr. Mikovits reported that the negative studies were due to researchers using a clone that was not representative of the variability found in the range of MLV’s present in ME/CFS. These clones, to my knowledge, are used in some studies to determine the sensitivity and specificity of the assays. Up until recently researchers were using what they had which were clones that referenced the original prostate cancer XMRV tissues. (See A New Kind of XMRV for more). Dr. Mikovits reported that the DHHS group is incorporating more variability into their search XMRV.
CDC – The CDC representative at the Press Conference, Dr. Monroe, did not concede the battle to the Lo/Alter group stating that his group, too, had looked for other MLV’s and had, in fact, found them in some prostate cancer patients but had found no evidence of them in its CFS study. (Besides the standard gag sequence, the CDC searched for XMRV and all possible MLV’s using the pol sequence and failed to find evidence of either of them. Since that sequence rarely changes across viral variants that test, hypothetically, should have picked up any MLV’s present but it did not. )
Is it the Cohorts After All? – An FDA FAQ paper just released specifically addressed the disparity between the CDC and FDA/NIH studies results. It suggested that methods in sample preparation may play a role and provided data indicating that the CDC and NIH cohorts may have been different.
Both labs were equally able to detect XMRV in positive (presumably spiked) samples provided by the DHHS Blood Working Group. Dr. Katz showed a slide at the CAA webinar indicating that all the participating labs, the CDC, BSRI, WPI, FDA were equally adept at detect XMRV in spiked samples. Positive patient samples are a different story, however, because they may contain variants of XMRV; every lab appears to be able to find XMRV in a spiked sample – a labs ability or inability to detect it in patient samples is the crux of the issue, right now).
Oceanblue on the Forums pointed out that Dr. Alter only referred to XMRV but said nothing about whether his lab found MLV’s in the CDC samples sent him. Did the Alter/Lo group find MLV’s in the XMRV negative CDC patients? If the answer to that question is ‘No’ that will indicate that cohorts may play a big factor in who has the bug(s).)

The two groups of patients were certainly very different. Twenty-five of the Alter study participants were provided by Dr. Komaroff from patients at his clinic. (Twenty-four tested positive. About 80% of them meet the Fukuda criteria while all met the Holmes criteria.) The rest came from Dr. Bell’s/Dr. Cheney’s practice.(8/12 positive)(Thanks to Ixcheli for the clarification).
The CDC study patients were picked up by random sampling and somewhere around half of them had never seen a physician for their illness. (Dr. Komaroff noted that some of the patients in the ‘other’ studies were not the kind of patients that came by his door). The CDC samples came from patients diagnosed using the Fukuda and/or Empirical Definitions – all of whom appear to have the meet Empirical Definition. The Empirical definition increased prevalence rates dramatically and ushered in a new breed of ‘CFS’ patient.
Dr. Alter later stated that geographical variations in the variants may play a role “There may be a geographic difference,” Dr. Alter told Medscape Medical News. “In the Northeast, CFS may be due to MLV, and in the West, it may be due to XMRV.”
It’s hard to imagine, though, that the cohort selection will explain some of the other negative studies. Dr. Huber reportedly used patients provided by Dr Levine in the US and some of the patients in the Groom study were provided by Dr. Kerr. We don’t know about the negative Joliceur study that has yet to be published but it seems likely, given his pro-CFS stance, that he used patients from CFS clinics. The WPI was also able to detect 2/7 positives in a Kuppeveld study that used the Oxford definition and who’s patient makeup appeared very unCFS-like. The findings do, however, indicate that patient selection can play a major factor in some studies. The CDC is reportedly preparing a paper on its results from a more severely ill ME/CFS.
The other factor the FDA response cited was differences in sample preparation. Since that’s all they stated its difficult to know what they were referring to. The Alter/Lo group found that testing plasma cut their positive rates in half compared to whole blood. The CDC used plasma – but so did the WPI in the original Science paper – and they, of course, had results similar to the Alter/Lo study. The FDA response did not, interestingly, suggest that they believed other problems with methodology played a role. However, the Alter/Lo paper discussed primer problems which may be similar to those Dr. Mikovits referred to in her video.
Contamination – the contamination question apparently still lingers in some sections of the research community and it will probably continue to linger as long as different labs get different results. There are very strong arguments against the possibility of contamination – the antibody results, the ability to grow the virus, the ability of the virus to infect other cells shown in the Science paper, and now the Alter papers findings. The Alter group went to great lengths to ensure contamination was not an issue and their ability to pick up mutated MLV’s in the same patients 15 years later was yet another strong argument against contamination yet at least some in the research community want more proof.
The editors of PNAS, however, wanted the Alter/Lo group to show evidence that the MLV’s they found were integrated into the human genome – that is, that the virus had inserted itself into a cell’s DNA. Because a contaminant is not a virus – it’s a genetic sequence from a virus – it could not actually infect a cell. (The WPI went so far as to show that the XMRV they found was able to transfer itself from one cell to the other.). The Alter/Lo group did not do that, citing the difficulty of having to wade through from hundreds to 1,000’s of cells in order to find the one infected with MLV’s.
Not a Breakthrough But a BIG Step Forward: While the Alter/Lo paper has been touted as a breakthrough it’s probably better thought of a big step forward. It will certainly provide much needed impetus for further study and some breathing room for the WPI and XMRV but until researchers can reconcile their results; ie until they can figure out who is doing what incorrectly – many will probably remain on the fence. Indeed, both the Alter group and the CDC indicated they are looking to the DHHS Blood Working group to reconcile their differences.
The second positive study did prompt more calls for anti-retroviral trials. Indeed a successful blinded, placebo-controlled anti-retroviral trial would settle the issue immediately. Several pharmaceutical companies interviewed, however, did not appear ready to put their money into an expensive study until more results had come in. That might not be a bad outcome given the quite variable results heard from patients. Andrea Whittemore is certainly doing something right and Dr. Deckoff and her daughter have significantly improved but one patient reported Dr. Peterson told him he had seen few success stories (altho other reports are of at least a dozen patients experiencing significant positive effects) and it’s still not clear which anti-retroviral drugs or drug combinations work best with XMRV.
The most basic question that remains unanswered is why the Lo/Alter group was able to look for and find the same genetic sequences that all the other failed studies had looked for. Dr. Alter and Dr. Lo had no specific answer to that question in the Press Conference – other than to note that the very low viral numbers made finding the retroviruses exceedingly difficult. They also noted that CFS, as currently defined, is a ‘spectrum disorder’ that probably incorporates many different subsets. There are also possible problems with the primers. Dr. Alter reported his lab is currently examining 1000 healthy blood donors and he is extending his search for MLV’s into a number of autoimmune and other disorders.
Conclusion: the Alter/Lo study validated the central finding of the WPI’s Science paper – that retroviruses are found in a high percentage of ME/CFS patients and in a low percentage of health controls. Some ancillary questions remain to be resolved including what types of MLV’s are present in ME/CFS and in what types of patients and all the researchers agreed that the Alter/Lo study indicated the need for much more extensive research. All looked to the DHHS Blood Working Group to resolve the essential questions about the virus and we await Dr. Vernon’s and Dr. Racaniello’s take on this fascinating study. More positive studies are reportedly on the way.
A Look at Dr. Alter
Possi bly the most influential researcher ever to publish on ME/CFS Dr. Harvey Alter is currently the chief of the infectious disease division of the Department of Transfusion Medicine at the NIH.
bly the most influential researcher ever to publish on ME/CFS Dr. Harvey Alter is currently the chief of the infectious disease division of the Department of Transfusion Medicine at the NIH.
Lasker Award: in 2000 he won the most prestigious award in medicine, the Lasker Award , for his work in discovering the hepatitis C. virus and in reducing the risk of getting a virus through a transfusion. Often referred to as the Nobel Prize of medicine 62 recipients of the Lasker award have gone on to win the Nobel Prize.
Getting a blood transfusion in the 1960s was remarkably risky with 30% of transfusion recipients becoming infected with hepatitis. Dr. Alter’s groundbreaking longitudinal studies indicating the hepatitis risk was largely associated with paid blood donors lead the FDA to institute an all volunteer blood donation system, cutting the infectious rate dramatically.
Next, his assertion that a mysterious virus he called non-hepatitis A/non-hepatitis B set was still infecting blood transfusion recipients and causing cirrhosis of the liver in 20% of those infected set off a massive hunt by dozens of labs. It wasn’t until Chiron Lab used new cutting-edge techniques that allowed them to sift through tens of millions of samples that the virus was finally identified as hepatitis C in the 1980’s.
Dr. Alter’s work ultimately lead to breakthroughs that reduced the infection rate of hepatitis through transfusion to essentially 0%. A prolific researcher, Dr. Alter has over 250 publications to his name. This year he has published four papers on XMRV, chronic HBV and HCV infections, parvovirus B19 (which is also associated with CFS), and interferon alpha.’
