Nature, (the second most read Science Journal in the world, published a long article on the search for XMRV. I think it’s pretty even handed. The article clearly outlines Dr. Mikovits commitment to the patients (and their commitment to her), gives us some idea why Dr. Peterson left, reviews the contamination issues, tells us that a true replication study by Dr. Levy is in the works, reports that a ‘next-generation DNA technique’ found XMRV and even mentions Phoenix Rising :)
When Judy Mikovits found links between chronic fatigue syndrome and a virus, the world took notice. Now, she’s caught between the patients who believe her work and the researchers who don’t.
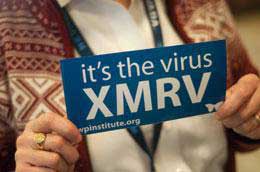
On a sunny January afternoon in Santa Rosa, California, a small crowd waits patiently for Judy Mikovits to arrive. She is scheduled to deliver a talk on a mysterious virus called XMRV, which she believes underlies chronic fatigue syndrome. Although she’s two hours late — held up by fog at San Francisco International Airport — not a single person has left. And when she arrives, they burst into applause.
To a rapt audience, she gives a chaotic and wide-ranging talk that explores viral sequences, cell-culture techniques and some of the criticisms that have been thrown at her since she published evidence1 of a link between XMRV and chronic fatigue in 2009. Afterwards, Mikovits is swarmed by attendees. A middle-aged woman who spent most of the talk in a motorized scooter stands up to snap pictures of her with a digital camera. Ann Cavanagh, who has chronic fatigue and has tested positive for XMRV, says that she came in part for information and in part to show her support for Mikovits. “I just wish there were a hundred of her,” Cavanagh says.
 The event was “surreal”, says Mikovits, a viral immunologist at the Whittemore Peterson Institute for Neuro-Immune Disease (WPI) in Reno, Nevada. She is discomfited by the attention from patients, which at times borders on adulation. But her reception among scientists has been markedly cooler. Numerous follow-up studies have found no link between the virus and the disease; no group has published a replication of her findings; and some scientists argue that XMRV is an artefact of laboratory contamination. Now, even some of Mikovits’s former collaborators are having second thoughts.
The event was “surreal”, says Mikovits, a viral immunologist at the Whittemore Peterson Institute for Neuro-Immune Disease (WPI) in Reno, Nevada. She is discomfited by the attention from patients, which at times borders on adulation. But her reception among scientists has been markedly cooler. Numerous follow-up studies have found no link between the virus and the disease; no group has published a replication of her findings; and some scientists argue that XMRV is an artefact of laboratory contamination. Now, even some of Mikovits’s former collaborators are having second thoughts.
Mikovits has dug in, however, attacking her critics’ methods and motives. She says that their distrust of her science stems from doubts about the legitimacy of chronic fatigue syndrome itself. Chronic fatigue, also known as myalgic encephalomyelitis, affects an estimated 17 million people worldwide, but it is emely difficult to diagnose. Many with the disorder are told that their symptoms — which include exhaustion, joint and muscle pain, cognitive issues, and heart and respiratory problems — are psychosomatic. “I had no idea there was that much bias against this disease,” Mikovits says.
The stakes are high and many are taking the risks seriously. Several countries have barred people with chronic fatigue from donating blood in case the virus spreads (see ‘Something in the blood’). And the US government has launched a US$1.3-million study to investigate the link. Patients are already being tested for XMRV, and some are taking antiviral drugs on the assumption that the virus causes chronic fatigue by attacking their immune defences. Many say that such action is premature, but Mikovits is steadfast. “We’re not changing our course,” she says.
First findings
In October 2007, Mikovits attended a prostate-cancer meeting near Lake Tahoe, Nevada, where she met Robert Silverman, a virologist at the Cleveland Clinic in Ohio. Silverman co-discovered XMRV, which stands for xenotropic murine leukaemia virus-related virus2. While examining human prostate tumours, he and his collaborators found genetic sequences that resemble retroviruses found in the mouse genome. Like all retroviruses, XMRV rewrites its RNA genome into DNA on infection, then slips the DNA into the genomes of host cells. Ancient remnants of such viruses litter animal genomes. But the only active retroviruses conclusively linked to human disease are HTLV-1, which causes leukaemia, and HIV.
At the meeting, Silverman was presenting research linking XMRV to deficiencies in a virus-defence pathway. Mikovits recalled that the same pathway was weakened in some patients with chronic fatigue. She wondered whether the prostate-tumour virus could also be behind chronic fatigue. After the meeting, Silverman sent Mikovits reagents to test for XMRV.
The idea excited Mikovits, but she had other priorities. After stints in industry and at the US National Cancer Institute (NCI) in Maryland, she had recently joined the WPI to lead its research programme. The WPI was founded in 2006 by physician Daniel Peterson, an expert on chronic fatigue, and by Annette Whittemore, the wife of a well-connected Nevada businessman, whose daughter Andrea has had chronic fatigue for more than 20 years. The Whittemores spent $5 million establishing the WPI, and several million more to support Mikovits’s research, which has attracted few other grants.
At the WPI, Mikovits established a sample collection from Peterson’s patients and began screening it for signs of an infection. A litany of pathogens has been linked to chronic fatigue over the years, including Epstein-Barr virus, Borna disease virus, human herpes virus 6 and HTLV-2. None panned out. Still, the disorder bears some hallmarks of an infection. Many patients report acute illness before chronic symptoms appear, and their bodies often show signs of an immune system at war. The disease can also crop up in apparent outbreaks, including one characterized by Peterson near Lake Tahoe in the 1980s.
Just before Christmas 2008, Mikovits turned her attention to Silverman’s reagents. She and her postdoc, Vincent Lombardi, known as Vinny, asked a graduate student to test for XMRV DNA in white blood cells from some of the most seriously ill people being studied at the WPI.
The first try turned up just two positives out of 20. But by tweaking the conditions of the test, Mikovits says her team found XMRV in all 20. “Vinny and I looked at each other and said, ‘Well, that’s interesting’,” she says. They spent the next few weeks convincing themselves that they were onto something, and soon conscripted Silverman and Mikovits’s former mentor at the NCI, Frank Ruscetti, to help prove that XMRV infection was behind chronic fatigue.
“We really retooled our entire programme and did nothing but focus on that,” she says. They kept the effort under wraps, dubbing it ‘Project X’. Even Peterson and the Whittemores weren’t clued in. Mikovits says that the secrecy was necessary because her team also found XMRV in the blood of some healthy people, raising concerns about blood products. She hoped to build an airtight case because she worried that sceptical public-health officials would undermine her work.
In May 2009, the team submitted a paper to Science reporting the identification of XMRV genetic material in two-thirds of the 101 patients with chronic fatigue they had tested and in 3.7% of 218 healthy people. They also included data suggesting that infected white blood cells could pass the virus on to uninfected cells.
Reviewers wanted more evidence: a clear electron micrograph of virus-infected cells, proof that patients mounted an immune response to the virus, an evolutionary tree showing XMRV’s relationship to other viruses and the locations where viral DNA was integrating into patient genomes. Mikovits’s team went to work. “None of us took any time off, not even a weekend,” she says. They resubmitted the paper in early July with everything the reviewers had asked for, except the DNA integration sites, which many scientists consider a gold standard in proving a retroviral infection.
Later that month, NCI officials who had learned about the work invited Mikovits to give a talk at a closed-door meeting with other XMRV researchers and government scientists. “When I finished speaking you could’ve heard a pin drop,” she says. Mikovits says she thinks at least one of her manuscript’s reviewers was at the meeting, because soon after, she got a call from a Science editor. Their paper had been accepted.
Jonathan Stoye, a retrovirologist at the MRC National Institute for Medical Research in London, wrote a commentary about the paper for Science3. He had never heard of Mikovits, but Frank Ruscetti’s name on the paper gave him confidence, he says, and “if it were true, it was clearly very important”. Stoye’s co-author John Coffin, a retrovirologist at Tufts University in Boston, Massachusetts, says he was satisfied with the data and thought it was time to “let the field and public chew on them”.
The BBC, US National Public Radio, The New York Times, The Wall Street Journal and dozens of other news outlets covered the research. “Prostate cancer pathogen may be behind the disease once dubbed ‘yuppie flu’,” Nature announced on its news website the day the paper came out. Phoenix Rising, a forum for patients with chronic fatigue that has become a hub for all things XMRV, called the work a “game changer”, and patients flocked to learn more about a virus that they hoped would explain their condition. But others, including Britain’s leading chronic fatigue patient group, urged caution until more research buttressed the link.
The first negative findings started to arrive in January 2010 — failing to find XMRV in 186 people with chronic fatigue from the United Kingdom4. A month later, a team including Stoye published a paper showing no evidence of XMRV in more than 500 blood samples from patients with chronic fatigue and healthy people. One day later, the British Medical Journal accepted a paper reporting more negative results in Dutch patients. Studies began piling up so fast that Coffin made a scorecard to show at talks. “I’ve lost count now,” he says.
Mikovits says that the discrepancies can be explained by differences in the geographical distribution of XMRV or in the methods used.
Judy Mikovits says that she will not abandon the hypothesis that XMRV and related viruses cause chronic fatigue syndrome, despite a growing chorus of critics.D.
The most common way to detect XMRV is PCR, or polymerase chain reaction, which amplifies viral DNA sequences to a level at which they can be identified. Mikovits and her team used this method to detect XMRV in some of their patients, but she contends that the most sensitive way to detect the virus is to culture patients’ blood cells with a cell line in which the virus replicates more quickly. This should create more copies of the virus, making it easier to detect with PCR and other techniques. She says that none of the negative studies applied this method exactly, a fact that annoys her.
In summer 2010, some evidence emerged in Mikovits’s corner. Harvey Alter, a hepatitis expert at the NIH’s Clinical Center, and his team identified viruses similar to XMRV in 32 of 37 people with chronic fatigue and in 3 of 44 healthy people. They were preparing to publish their results in the Proceedings of the National Academy of Sciences. But scientists at the Centers for Disease Control and Prevention (CDC) in Atlanta, Georgia, were about to publish a negative report. The authors delayed publication of both papers for several weeks to assess discrepancies. The move agitated Mikovits as well as the chronic-fatigue community, who suspected that important data were being suppressed.
When Alter’s work came out in late August7, Mikovits was ecstatic, and the WPI released a YouTube video of her touting it. For other researchers, however, the new paper had shortcomings. The viral sequences from Alter’s paper differed from XMRV, says Greg Towers, a retrovirologist at University College London. “He doesn’t get variation, he gets a totally different virus.” Towers says that mouse DNA, which is chock-full of virus sequences like those Alter’s team found, probably contaminated their samples, which were collected in the 1990s. But Alter says that his team found no contamination from mouse DNA and recovered the same viral sequences from the same patients sampled a decade later.
Contamination became a dirty word for Mikovits. Just before Christmas 2010, Retrovirology published four papers9,10,11,12 that highlighted laboratory contamination as a possible explanation for her findings. One showed, for example, that mouse DNA contaminates an enzyme from a commercial kit commonly used for PCR. Coffin, an author on two of the Retrovirology papers, urges caution against over-extrapolating. These papers do not say that contamination explains Mikovits’s results, he says, just that extreme care is required to avoid it.
Towers and his colleague Paul Kellam, a virologist at the Wellcome Trust Sanger Institute near Cambridge, UK, are less charitable, however. Their study12 showed that the XMRV sequences that Mikovits and Silverman had extracted from patients lacked the diversity expected of a retrovirus that accumulates mutations as it passes between patients. “This doesn’t look like an onwardly transmittable infectious virus,” says Kellam. A press release for the paper issued by the Sanger Institute put it more bluntly: “Chronic fatigue syndrome is not caused by XMRV.”
Mikovits is riled when the topic turns to Towers’s paper over dinner one night in Reno — “Christmas garbage”, she calls it. Contamination cannot explain why her team can reproduce its results both in her lab in Reno and at Ruscetti’s at the NCI, she says. Her team checks for contamination in reagents and in the cells it grows the patients’ samples with. She says that her team has also collected viral sequences that will address Towers’s and Kellam’s criticism but that it hasn’t yet been able to publish them. Meanwhile, an unpublished study of patients in Britain with chronic fatigue bears out the link to XMRV, she says. “I haven’t for one second seen a piece of data that convinced me they’re not infected.”
Jay Levy, a virologist at the Univer*sity of California, San Francisco, has a window in his closet-sized office that looks out into the laboratory where, in the 1980s, he became one of the first scientists to isolate HIV. After his discovery was scooped by other researchers, Levy turned his attention to chronic fatigue and started a long but fruitless search for an infectious cause.
Now, Levy is putting the finishing touches on what could be the most thorough response yet to Mikovits’s Science paper, adopting the same cell-culture techniques to detect the virus and using samples from the same patients. He’s done this with the help of Daniel Peterson, who left the WPI in 2010 for what Peterson says are “personal reasons”. Peterson has questioned the institute’s singular pursuit of XMRV, a research direction that was pursued without his consultation.
Mikovits says that she kept the XMRV work secret from Peterson over fears he would tell his patients, and left his name off the original Science manuscript until a reviewer questioned the omission. When asked whether that episode contributed to his departure, he says, “I was surprised at the secrecy and lack of collaboration.” As for his motivation to team up with Levy: “I’m just trying to get to the truth. It’s my only motive, because this is such a deserving group of patients who need to know what’s going on.”
Others, too, are rallying for a definitive answer. Ian Lipkin, a microbial epidemiologist at Columbia University in New York, has a reputation for getting to the bottom of mysterious disease–pathogen links. His team debunked the association between Borna disease virus and chronic fatigue, for example. Now he is spearheading the $1.3-million effort funded by the US government. He is leaving the testing to three labs: Mikovits’s at the WPI, Alter’s at the NIH and the CDC. Each will receive coded samples of white blood cells and plasma from 150 patients with chronic fatigue and from 150 healthy controls. The labs will test for XMRV using their method of choice. Lipkin will crunch the data and unblind the samples.
But even if a study confirms the link to chronic fatigue, it won’t be able to determine whether the virus is the cause. XMRV could, for example, be an opportunistic infection affecting those whose immune systems are already dampened by chronic fatigue. Even Mikovits can only hypothesize as to how it might cause disease.
The virus might not even exist as a natural infection. At a retrovirus conference this month in Boston, Massachusetts, Coffin and his colleague Vinay Pathak at the NCI in Frederick, Maryland, presented data showing that XMRV emerged in the 1990s, during the development of a prostate-tumour cell line called 22Rv1. Developing the line involved implanting a prostate-tumour sample into mice, retrieving cells that might divide indefinitely and repeating the process. But looking back at DNA samples taken throughout the cell-line’s development showed that human cells became infected only after passing through several different mice. Importantly, XMRV’s sequence seems to have come from two different mouse strains. “They just sort of snapped together like two puzzle pieces,” says Coffin, an event extremely unlikely to have happened twice.
XMRV sequences retrieved from patients with prostate cancer and chronic fatigue — including some who have had chronic fatigue since the mid-1980s — are nearly identical to the virus from 22Rv1 cells. The implication, says Coffin, is that this virus, born in a laboratory, has probably been infecting samples for more than a decade, but not people. “Although people on the blogs aren’t going to believe me, I’m afraid this is by far the most reasonable explanation for how XMRV came to be,” says Coffin, who hoped that the association with chronic fatigue would pan out and still thinks some pathogen other than XMRV could explain the disease.
Silverman, who no longer works with Mikovits, says that he wasn’t using 22Rv1 cells when XMRV was discovered. Nonetheless, the work has rattled his confidence in XMRV’s link to both prostate cancer and chronic fatigue.
Mikovits, however, is undeterred. The WPI owns a company that charges patients up to $549 to be tested for XMRV, and Mikovits believes that patients who test positive should consult their doctors about getting antiretroviral drugs normally prescribed to those with HIV. Levy and others worry that she is overreaching. “That’s scary for me. These antiretroviral drugs are not just like taking an aspirin,” he says. Mikovits argues that they might be some patients’ only hope. “The people who we know they’re infected should have a right to get therapy,” she says, “They have nothing. They have no other choice.”
Context and debate
Back in her Reno laboratory two days after the talk in Santa Rosa, Mikovits examines a stack of small plastic flasks under a microscope. Some contain patient cells that she hopes will turn into cell lines and churn out XMRV. “On Wednesdays I get to take care of my cells, and that’s where I’m the happiest,” she says.
She has just come off the phone from a sobbing patient infected with XMRV whose symptoms had worsened.
Mikovits clearly shares in the frustration of those with chronic fatigue who have been marginalized over the years and told that their disease is not real. She says that this disbelief in the disorder drives the criticism of her work. Kellam and the others say that this isn’t true. They don’t deny the existence of the syndrome or even the possibility of an infectious origin. “What we’re trying to understand is the aetiology,” Kellam says. “It’s a scientific debate.”
Mikovits says that she’s analysed all the papers critical of her work and found flaws in each of them. Nevertheless, she’s quick to endorse findings that support her work. She claims that Coffin and Pathak’s study, for example, “says nothing about human infection”. Yet new work presented at a different meeting that found XMRV using next-generation DNA sequencing offers “no doubt it’s not contamination — that the whole story’s real”, she says.
Despite the growing choir of sceptics, Mikovits says that she has simply seen too many data implicating XMRV and other related viruses in chronic fatigue to change her mind. For her supporters, that steadfastness offers legitimacy and hope. “The scientists are moving forward,” she announced at her talk in Santa Rosa, “and I think the politics will go away shortly.” The crowd responded with vigorous applause.
Ewen Callaway writes for Nature from London.
