Discuss this article on the forums
(The repeat exercise tests for ME/CFS developed by Staci Stevens are beginning to transform the research field with growing numbers of researchers understanding that the abnormalities of ME/CFS patients reveal themselves fully only when they are put under stress. Phoenix Rising has been graced by two series of articles elucidating different aspects of the all important post-exertional-malaise (PEM) experienced in ME/CFS; Jennie Spotila’s four part series and now Lannie’s personal account of her repeat exercise tests and what she learned from them.
You can find Lannie’s original blog here as well as blogs on her treatment for Lyme disease and other topics).
The Stevens’ Protocol – PART 1

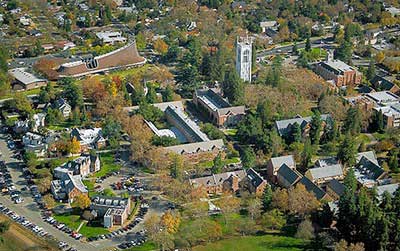
November 1st and 2nd, I traveled to Stockton, CA to the University of the Pacific Department of Sports Sciences Fatigue Lab. There, I underwent a 2-day Cardiopulmonary Exercise Stress Test, also known as the Stevens’ Protocol. The test was created by Staci Stevens, MA, the Founding Executive Director of the Pacific Fatigue Laboratory.
The Stevens’ Protocol is THE gold standard in diagnosing, and therefore proving Chronic Fatigue Syndrome(CFS) disability. And more specifically, proving the universal CFS symptom of post exertional malaise (PEM). As talked about extensively at the CFSAC meeting in DC, CFS is made up of a laundry list of possible symptoms. The one universal symptom, however, is post exertional malaise. Pacific staff admit that to date many of their patients have been referred to the University of the Pacific by disability attorneys, as it’s been found extremely helpful in disability cases.
The premise of this test is to put the person with CFS (PWC) under a traditional exercise stress test, which most PWCs can suffer (if barely) through. The differentiating factor in the Stevens’ protocol is they ask the PWC to return and repeat the test exactly 24 hours later. It’s during this day 2 when the markers tank, and her team can prove disability. The way I like to put it is, “sure, maybe I could suffer through a half-day of work(ie. day 1), but if I have to return any earlier than 10 days later (ie. day 2) you’ll have to take me out on a gurney” type proof.
 In addition to providing proof of disability, the protocol provides patients with a key piece of information – their anaerobic threshold (AT). Stevens believes it’s when a PWC repeatedly moves from their anaerobic to aerobic heart rate levels, they bring on crashes and more severe crashes. Athletes utilize knowledge of this AT level all the time to optimize their training, as when you move into your aerobic heart rate you begin oxygen deprivation and workouts become less efficient. Same for PWCs, except think of it as our daily energy envelope gets smaller in addition to depriving our already foggy brains of oxygen. Her recommendation is to identify your AT, wear a heart rate monitor, and then start to learn what causes your heart to increase. When it goes to or above your AT, stop what you’re doing and allow it to return to your resting heart rate.
In addition to providing proof of disability, the protocol provides patients with a key piece of information – their anaerobic threshold (AT). Stevens believes it’s when a PWC repeatedly moves from their anaerobic to aerobic heart rate levels, they bring on crashes and more severe crashes. Athletes utilize knowledge of this AT level all the time to optimize their training, as when you move into your aerobic heart rate you begin oxygen deprivation and workouts become less efficient. Same for PWCs, except think of it as our daily energy envelope gets smaller in addition to depriving our already foggy brains of oxygen. Her recommendation is to identify your AT, wear a heart rate monitor, and then start to learn what causes your heart to increase. When it goes to or above your AT, stop what you’re doing and allow it to return to your resting heart rate.
I learned about the Stevens’ Protocol when I first was sick with CFS, filed it away in my foggy mind, and moved on. Recently it seemed as if I saw it referenced everywhere, especially on the Phoenix Rising forum. And then again by Dr. Christopher Snell at the CFSAC meeting in DC this October. I am at the third stage of my SSA case, so could use more substantiation. I also really liked the AT theory, and wanted to understand how I could control my energy better by eliminating crashes. So, I decided to really look into it.
I called the University and talked to an undergraduate student who assists in the Fatigue Lab. He emailed me the packet I’d need to fill out, should I decide to have the test done. It included the doctor referral forum I’d need my doctor to sign and fax back, as well as pricing breakdown and patient requirements. The test is $2,000, and I was really only willing to do it if my insurance paid for some of it. He was also kind enough to send me a copy of an old invoice that broke the test down into individual procedures and costs along with the appropriate procedure codes. I was able to use these procedure codes to call my insurance (Cigna PPO) and determine if they covered this test. They said they covered each and every one. (Note: I had to pre-pay for the test out of pocket, and have only just submitted the claim to insurance today. I’m confident they will cover each of the procedures once. However, I’m unsure if they will pay for the repeat. As soon as I have this information I’ll share.)
PRICING
Day 1, Cardiac Stress Test, CPT Code 93015, $329
Day 2, Cardiac Stress Test, CPT Code 93015, $329
Day 1, CO2/O2 Analysis, CPT Code 94681, $188
Day 2, CO2/O2 Analysis, CPT Code 94681, $188
Day 1, Oxygen Saturation w/Exercise, CPT Code 94761, $71
Day 2, Oxygen Saturation w/Exercise, CPT Code 94761, $71
Day 1, Spirometry (baseline), CPT Code 94010, $76
Day 2, Spirometry (baseline), CPT Code 94010, $76
Day 1, Flow Volume Loops, CPT Code 94375, $84
Day 2, Flow Volume Loops, CPT Code 94375, $84
Day 1, MVV(Max Vol Ventilation), CPT Code 94200, $34
Day 2, MVV(Max Vol Ventilation), CPT Code 94200, $34
Day 1, Nasal Acoustic Rhinometry, CPT Code 92512, $59
Day 2, Nasal Acoustic Rhinometry, CPT Code 92512, $59
Day 1, Nasal Acoustic Rhinometry, CPT Code 92512, $59
Day 2, Nasal Acoustic Rhinometry, CPT Code 92512, $59
Day 1, Cal Cap Reaction Time, CPT Code 96103, $100
Day 2, Cal Cap Reaction Time, CPT Code 96103, $100
PATIENT REQUIREMENTS
- Ability and willingness to provide an excellent effort for both exercise tests (Note: they can actually tell by your results if you “tried.” Based on your “RQ” or Response Quotient or Oxygen to Carbon Dioxide ratio. I’ll talk more about this in Part 2)
- Someone to accompany you to and from the Pacific Fatigue Laboratory
- Classification as low to moderate risk for cardiovascular disease
- Consideration for using test results for research purposes. All results will remain completely confidential
- Completion and return of the following forms:
- a. Physician referral for testing
- b. Cardiovascular Risk Stratification Form
- c. Informed consent for testing and/or consent for research
- d. Medication list
Photo sources: The University of the Pacific
